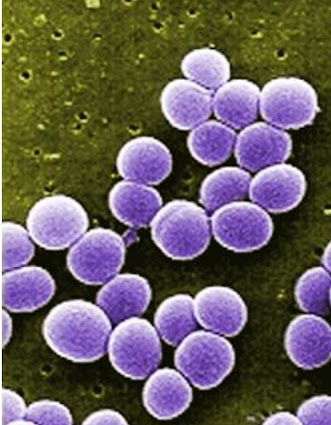
Listeria monocytogenes, a bacterium with deadly implications, poses a significant risk to public health. This organism is not to be underestimated, as it can lead to severe conditions such as encephalitis, meningitis, blood-borne infections, and ultimately, death. Its potency is particularly alarming for vulnerable populations, including pregnant women, newborns, the elderly, and individuals with weakened immune systems. Shockingly, Listeria accounts for approximately 28% of fatalities attributed to foodborne illnesses.
What makes Listeria monocytogenes especially menacing is its remarkable resilience in adverse conditions. Unlike many bacteria, it can endure acidic environments, high levels of nitrites and salt, and even survive in refrigerated temperatures. Consequently, it proliferates in various food sources, with raw (unpasteurized) milk, soft-ripened cheeses like Brie, and ready-to-eat meats such as hot dogs and pâté being common breeding grounds. Moreover, its reach extends to raw and smoked fish, poultry, fresh produce, and even ice cream.
The insidious nature of listeriosis, the infection caused by Listeria, adds to its danger. Symptoms initially manifest as seemingly benign, including headaches, low-grade fevers, muscle aches, nausea, and vomiting. Regrettably, these signs often mimic those of viral illnesses, leading to misdiagnosis and delayed treatment. Such delays offer Listeria the opportunity to progress unchecked. Furthermore, symptoms may not surface until anywhere from 3 to 70 days after exposure, further complicating detection and intervention.
Treating Listeria infections demands a proactive approach. Injectable antibiotics such as penicillin, ampicillin, or gentamicin, as well as intravenous trimethoprim/sulfamethoxazole, are essential for combating the bacterium. However, prevention remains the most effective defense. Individuals at heightened risk should steer clear of foods prone to harboring Listeria or ensure thorough cooking until piping hot (at least 180 degrees Fahrenheit) before consumption.
In conclusion, understanding the multifaceted threat posed by Listeria monocytogenes is paramount to safeguarding public health. By recognizing its resilience, insidious onset, and the necessity for preemptive measures, we can mitigate its devastating impact and protect vulnerable populations from its pernicious effects.
Understanding the Threat of Listeria monocytogenes
White Castle: The Birth of America's Iconic Fast-Food Hamburger
-
White Castle, an iconic American fast-food chain, was founded in Wichita,
Kansas, in 1921 by Walter (Walt) A. Anderson and Billy Ingram. At the time,
Ameri...